Rapid tests that call for nasal swabbing are not designed to collect and analyze your saliva.
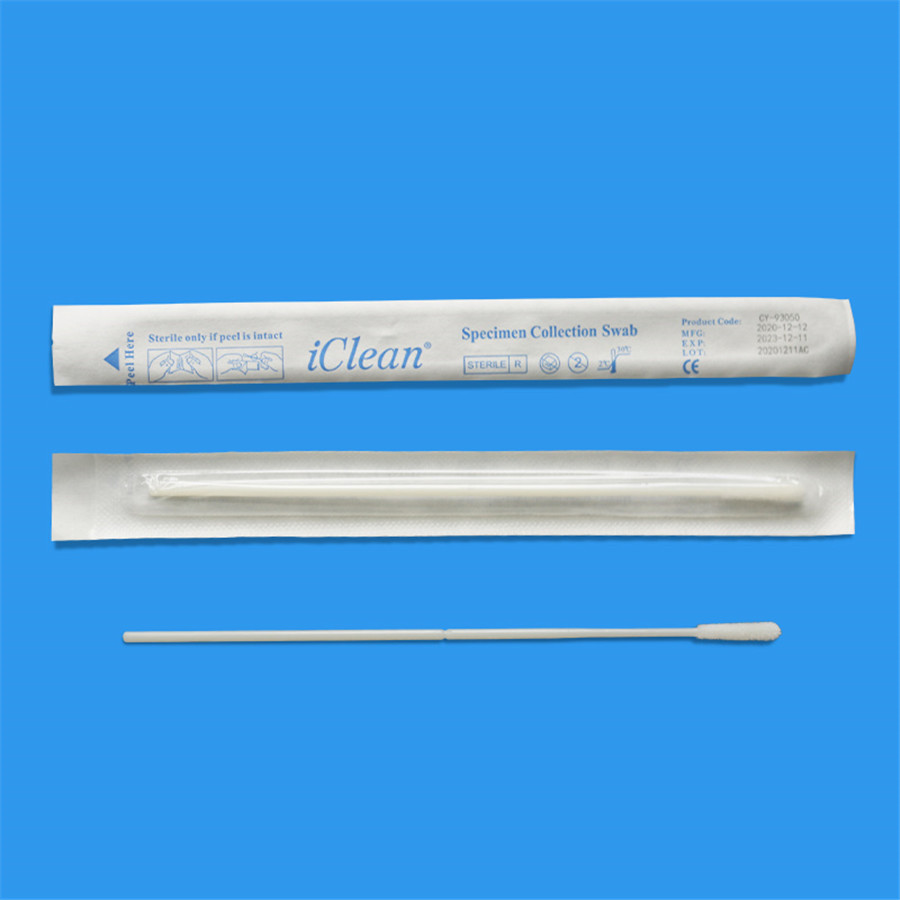
Is a throat swab or nose better for a COVID-19 rapid test? Some evidence suggests that obtaining a throat swab with an at-home antigen test might detect newer SARS-CoV-2 variants better than a nasal swab. For example, research has found that the Omicron variant is more detectable in saliva. Medical Swab
However, at-home tests are not designed for throat swabbing. As of 2023, the Food and Drug Administration has not approved the throat swab method for at-home antigen tests. The Centers for Disease Control (CDC) urges you to use those tests only as the instructions direct. That helps reduce your risk of an inconclusive or false result.
Still, some people have found swabbing their throats helpful. Read on to learn how a throat swab works, whether it detects COVID better than a nasal swab, and if it's safe.
At-home antigen tests direct you to perform a nasal swab to obtain a specimen sample. Some evidence suggests that using those tests to obtain a throat swab helps easily detect SARS-CoV-2 variants like Omicron.
It's essential to prepare your at-home antigen test properly, whether you do a nasal or throat swab. Start by making sure that your testing kit contains all of the materials listed and is not expired. Disinfect the area where you will lay out your testing kit. Wash your hands with soap and water, then remove the swab. Avoid touching the soft end.
Collect your specimen using a nasal swab or throat swab. Follow your testing kit's instructions for transferring your specimen to the provided solution. You'll need to wait about 20 minutes to read your results. Make sure that you dispose of all materials and wash your hands after you are done.
Here's how to obtain a nasal or throat swab:
There are benefits and risks of both nasal and throat swabs. It's essential that you consider both pros and cons before obtaining a throat swab with an at-home antigen test. Talk to a healthcare provider about the best COVID testing method for you.
A nasal swab might be more reliable than a throat swab. The Food and Drug Administration has approved the nasal swab method for at-home antigen tests. The CDC urges people to use at-home antigen tests as the instructions direct. Mishandling the testing kit might increase your risk of an inconclusive or false result.
In contrast, research has found that your nostrils do not carry as much of the virus as your saliva during the early stages of COVID. At-home antigen tests are generally less sensitive and have a higher rate of false negatives than other methods.
Swabbing your throat to obtain a test sample makes sense at face value. That's especially true if you are trying to capture as much virus as possible. Obtaining a throat and nasal swab with the same testing kit might provide more specimens for an accurate result.
Some evidence suggests that Omicron starts in the lower respiratory system and multiplies there 70 times faster than previous variants. That means viral material might not get to your nose as quickly as symptoms come on, Nathaniel Hafer, PhD, an assistant professor of molecular medicine at UMass Chan Medical School, told Health.
Still, more studies are needed to support the throat swab. It's unclear if at-home throat-swabbing may lead to false results, particularly when home users operate without a standard set of directions.
Other possible risks of using an at-home antigen test to obtain a throat swab include:
A throat swab might increase the sensitivity of an at-home antigen test, possibly making it more accurate than a nasal swab. The higher the sensitivity, the generally more accurate your results are.
For example, PCR tests, known as the "gold standard" for COVID tests, are more accurate in detecting COVID when using saliva samples than nasal ones. PCR tests are highly sensitive diagnostic tools that amplify viral genetic material to diagnose COVID.
"PCR tests are ultra-sensitive and pick up dead viral fragments even after you stop being contagious," Jennifer Lighter, MD, a pediatric infectious disease specialist at NYC Health + Hospitals/Bellevue, told Health. "Antigen tests are only positive when you're contagious, but their sensitivity is actually excellent when you're symptomatic or have had close exposure."
Still, the sample you use for testing has to be a good one. Antigen tests do not amplify viral genetic material in the same way that PCR tests do. It's unclear how human error might affect results when misusing at-home antigen testing kits.
A throat swab is generally safe if performed correctly but might have some risks. For example, doing a throat swab on yourself may be hard if you cannot get a good view of the back of your throat.
Certain side effects of a throat swab might worsen COVID symptoms like:
Of equal if not greater concern is the risk of reducing your test's accuracy, said Hafer: "There's a likelihood that it won't perform as indicated."
A false negative may create a false sense of security, leading you to spread the virus to others unknowingly. In contrast, you might get a false positive that contributes to unnecessary isolation and stress.
There are many ways to break the tests, said Hafer. One such way could involve saliva from a throat swab. The pH of the buffer is designed specifically for nasal swab specimens in at-home antigen tests. Adding saliva to the mix might contaminate your sample and interfere with test results, Clare Rock, MD, an assistant professor of medicine at the Johns Hopkins University School of Medicine, told Health.
The CDC advises using at-home antigen tests as the instructions direct. In a statement provided to Health, the Food and Drug Administration advised that "COVID tests should be used as authorized, including following their instructions for use regarding obtaining the sample for testing." As of 2023, the Food and Drug Administration has not approved the throat swab method for at-home antigen tests.
"Until there are more studies and the [Food and Drug Administration] and CDC revise their guidelines, my advice would be to follow all the instructions that come with an at-home antigen test, including how to swab," Jeffrey Dlott, MD, the medical director of Quest Diagnostics General Health and Wellness and Chronic Care Management services, told Health.
You'll want to take a COVID test right away if you have symptoms like a fever, cough, and sore throat. In contrast, the CDC advises that you wait five days to test if you had a possible COVID exposure. The CDC says that you need to test again 48 hours later if you test negative.
Isolate for at least five days if you test positive. Make sure that you wear a high-quality mask if you must be around others inside of your home. You may end your isolation after five days if your symptoms are going away and you do not have a fever for 24 hours without the use of a fever reducer.
Some people perform a throat swab to test for COVID at home using antigen tests. A throat swab is possibly better at detecting COVID than nasal swabs. Newer variants like Omicron are typically more detectable in your saliva than in your nostrils.
Still, the Food and Drug Administration has not approved the throat swab method for at-home antigen tests as of 2023. It's essential that you follow the instructions to lower your risk of an inconclusive or false result.
Goodall BL, LeBlanc JJ, Hatchette TF, et al. Investigating the sensitivity of nasal or throat swabs: Combination of both swabs increases the sensitivity of SARS-CoV-2 rapid antigen tests. Microbiol Spectr. 2022;10(4):e0021722. doi:10.1128/spectrum.00217-22
Jung EJ, Lee SK, Shin SH, et al. Comparison of nasal swabs, nasopharyngeal swabs, and saliva samples for the detection of SARS-CoV-2 and other respiratory virus infections. Ann Lab Med. 2023;43(5):434-442. doi:10.3343/alm.2023.43.5.434
Food and Drug Administration. SARS-CoV-2 viral mutations: Impact on COVID-19 tests.
Centers for Disease Control and Prevention. Self-testing at home or anywhere.
Centers for Disease Control and Prevention. How to collect a nasal mid-turbinate specimen for COVID-19 testing.
Food and Drug Administration. Pilot COVID-19 at-home test - instructions for use home testing.
Brooks ZC, Das S. COVID-19 testing.Am J Clin Pathol.2020;154(5):575-5doi:10.1093/ajcp/english141
Hui KPY, Ho JCW, Cheung MC, et al. SARS-CoV-2 Omicron variant replication in human bronchus and lung ex vivo. Nature. 2022;603(7902):715-720. doi:10.1038/s41586-022-04479-6
Hernandez MM, Riollano-Cruz M, Boyle MC, et al. Food for thought: Eating before saliva collection and interference with SARS-CoV-2 detection. J Med Virol. 2022;94(6):2471-2478. doi:10.1002/jmv.27660
El-Sharkawy F, Tang CN, Fitzgerald AS, et al. Saliva versus upper respiratory swabs: Equivalent for severe acute respiratory syndrome coronavirus 2 university screening while saliva positivity is prolonged after symptom onset in coronavirus disease 2019 hospitalized patients. J Mol Diagn. 2022;24(7):727-737. doi:10.1016/j.jmoldx.2022.03.012
Centers for Disease Control and Prevention. COVID-19 testing: What you need to know.
Healy B, Khan A, Metezai H, et al. The impact of false positive COVID-19 results in an area of low prevalence. Clin Med (Lond). 2021;21(1):e54-e56. doi:10.7861/clinmed.2020-0839
Patriquin G, Davidson RJ, Hatchette TF, et al. Generation of false-positive SARS-CoV-2 antigen results with testing conditions outside manufacturer recommendations: A scientific approach to pandemic misinformation. Microbiol Spectr. 2021;9(2):e0068321. doi:10.1128/Spectrum.00683-21
Food and Drug Administration. At-home OTC COVID-19 diagnostic tests.
Centers for Disease Control and Prevention. Isolation and precautions for people with COVID-19.

Nose Swab By clicking “Accept All Cookies”, you agree to the storing of cookies on your device to enhance site navigation, analyze site usage, and assist in our marketing efforts.